In what was anticipated to be a pivotal year for combating HIV, recent funding cuts have dramatically undermined HIV prevention and treatment initiatives across Africa. With decades of research culminating in promising breakthroughs, the rollout of new preventive drugs and vaccines faced an unexpected halt after substantial funding from the U.S. was withdrawn.
One of the most significant developments was the introduction of lenacapavir, a groundbreaking injection designed to provide strong protection from HIV, particularly for young women who have been disproportionately affected by the epidemic. Last year, about 300,000 young women were infected with HIV, making targeted prevention crucial. Health experts had envisioned a robust rollout of this drug throughout eastern and southern Africa.
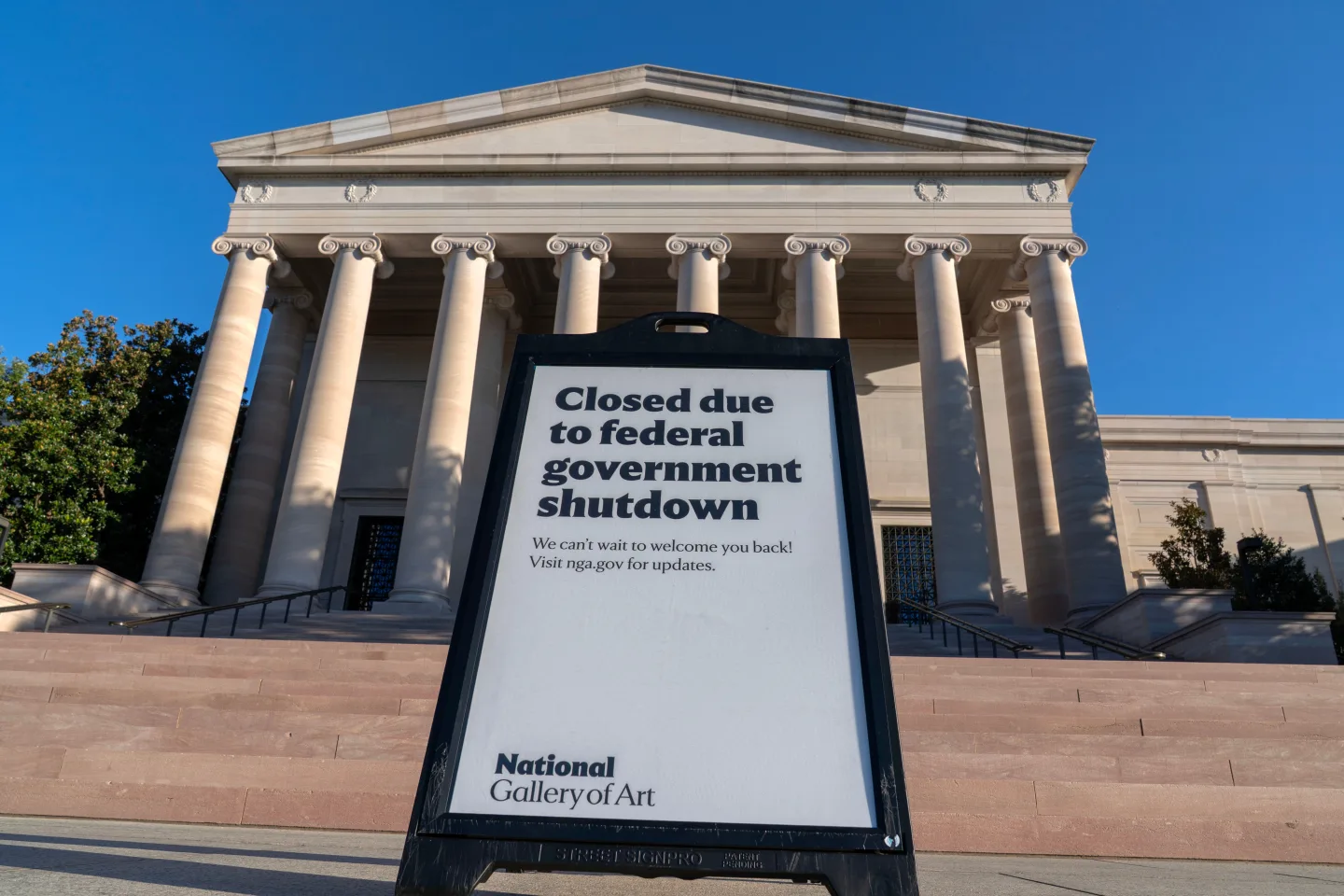
However, the ambitious plans encountered a major setback, largely attributed to the Trump administration’s reduction of foreign assistance. Healthcare providers across Africa are now grappling with a rapidly changing landscape. Clinics have become inaccessible, many outreach workers have lost their jobs, and a considerable number of individuals with HIV failed to collect their medications, jeopardizing efforts to control both the spread of the virus and the health of affected populations.
Dr. Leila Mansoor, a prominent research scientist focusing on HIV prevention in South Africa, expressed disappointment over the lost momentum in HIV research and preventative efforts. Plans to analyze HIV data, track the potential impact of lenacapavir, and conduct further trials have now been thrown into uncertainty.
While the scientific community remains hopeful and recognizes the potential to end the HIV epidemic, the challenge to navigate these funding deficits represents a significant barrier to achieving the envisioned public health goals. As program managers scramble to find alternative funding sources, the stakes could not be higher for millions depending on effective HIV prevention and treatment.